In previous articles we have considered the raft of changes in legislation and regulation that have affected the operation of GP practices in the UK. These changes have undoubtedly added to the pressures felt by UK GPs and Practice Managers and created significant fears for the future of GPs as the principal providers of primary care in the UK. But how do UK GPs really feel about the changes that have been imposed on their practice?
A recently published survey by the BMA answers this question and will make gloomy reading for those who have a vested interest in the future provision of a thriving, confident and optimistic GP-led primary health care service.
The Survey
A BMA quarterly tracker survey, conducted by its Health Policy and Economic Research Unit between July and August 2014 and sent to over 1,000 medical practitioners, revealed significant disparities within the profession regarding their levels of moral and their perceptions of their work-life balance.
The survey involved practitioners at Consultant, GP, SAS (Staff and Associate Specialists) and Junior Doctor in training level, together with a small group of “others”. Some of the responses make stark reading for GPs.
The principal findings, in so far as they relate to the position of GPs within the NHS, can be summarised as follows:
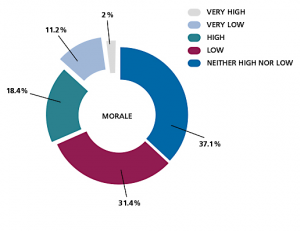
GP Morale
In excess of 40% of participants in the survey expressed their morale to be either low or very low. The same percentage said that morale was moderate, with only 20% indicating that it was high or very high. A dissection of these figures across the various disciplines reveals that GPs reported a lower average morale than the other areas of practice surveyed and, equally worrying, a marked drop in morale amongst junior doctors when compared to previous quarters.
Work/Life Balance
Not surprisingly, the findings regarding levels of morale were closely reflected in those that related to work/life balance. Once again, GPs reported the lowest average levels of contentment with their work/life balance, whilst the responses of junior doctors mirrored those related to morale – a noticeable reduction since the previous quarter. The figures also revealed a close correlation between the requirement to work outside normal hours and dissatisfaction with the work/life balance.
Workloads
Whilst the overwhelming majority of doctors report working outside their regular hours, once again GPs indicated the greatest concerns, with almost three quarters admitting that they were unlikely to be able to manage or sustain their existing workloads, with GPs also being the most likely to report that they were ‘always’ working beyond their regular hours during the course of the previous month. The reasons given for the need to do so were cited, in order, as excessive amounts of work and staffing shortages/unfilled vacancies.
Future Plans
Only approximately 25% of those surveyed experienced feeling satisfaction with their careers, with 44.2% of GPs being the most likely to consider taking early retirement. Once again, GPs feature the highest in terms of thinking about prematurely leaving the service.
Entering the Profession
In terms of the factors influencing the decision as to whether to go into the profession, the factors most likely to contribute were reported as being working hours, working conditions and ongoing changes to the NHS.
Summary
The survey goes on to deal with other matters that are beyond the scope of this article but the issues that we have covered clearly demonstrate a general feeling of demoralisation, dissatisfaction and insecurity amongst GPs, which is likely to have been worsened by the recent publication of the Five Year Forward Review.
What is clear is that GPs and their Practice Managers will have to investigate and implement every available strategy if they are to meet the present and future challenges facing GP practices in the UK.
Contact us to discuss how TrainingPrimaryCare can help your practice, CCG or Federation. Telephone 0203 174 0888 or email support@thetrainingnet.com
Previous news items