Let’s face it, it’s not going to happen. We all hope it will, but it won’t. We’ll have to soldier on.
There ain’t goinna be a merger of the NHS and social care any time soon. Sure, there will be a Green Paper and we should all pay attention and have our say but the reality is; there are is an insurmountable problem.
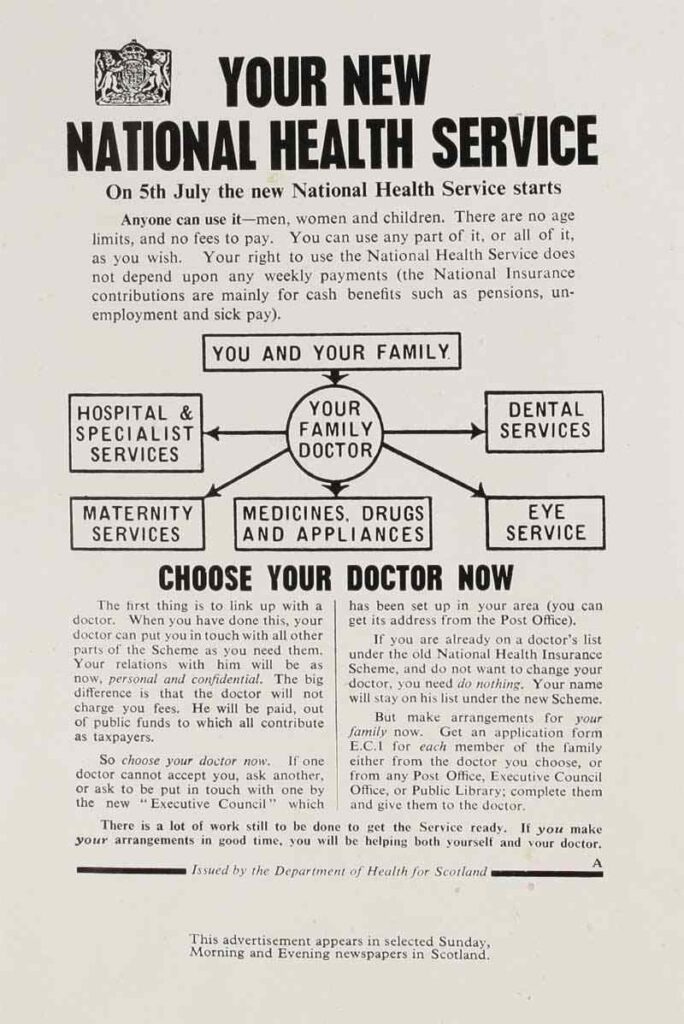
NHS care is free at the point of need. The introductory leaflet, posted to every house-hold, back in July 1948, announcing the NHS, page one, paragraph one, said this:
‘The NHS will provide you with all medical, dental and nursing care. Everyone, rich or poor, man, woman or child – can use any part of it. There are no charges…’
… and, more or less, with the exception of prescription, eye tests and some ancillary charges, it’s stayed like that for 70 years.
In the NHS’ 70th anniversary year, the government won’t unpick that. You get what you need and you don’t have to pay.
It’s important. Why?
… because social care is means tested. You pay for what you need, until you can’t pay.
Actually, it’s worse than that. Providers of adult social care, local authorities, do their own thing.
Where you live is what you get. In England there are 27 county councils, 201 district councils, 32 London boroughs, 36 Metropolitan Boroughs, 55 Unitary Authorities, plus the City of London.
Some of these, run adult social care services, some don’t. However, they are entwined. There are 18,100 councillors in England, each with their own view of who gets what.
The Care Act, that must be read in conjunction with chunks of other legislation, says eligibility assessments have to be carried out. They must involve the person and meet the national minimum, ‘Fair Access to Care’, eligibility thresholds. It’s a nonsense.
This is what CarersUK have to say:
‘This system of bands at low, moderate, substantial and critical risk is known as Fair Access to Care Services. Local authorities set their own policies on what band they will provide care at.
For some local authorities those with only critical needs will receive social-care but in the majority, only those with substantial needs will qualify for support….’
Merging that lottery with antithetical NHS legislation and objectives is the problem.
Does social care become free at the point of need or does healthcare come at the whim of local social services? Health run by Councillors.
In the meantime, yer granny will still have to flog her house to pay for her care.
Looking forward… none but the really lucky millennials will be able to afford a house. The rental market will look like France and Germany. They’ll have no home to flog, to pay for their care.
Any solution has to involve upping taxes across the board.
In the meantime at the front-line, we will have to look at what works. How health and social care work better together.
In my travels… there are four things that stand out.
The first; Proximity pays.
Wherever there is an actual social services person with a desk and a computer plumbed into a working ward, discharges work better. Being part of the team, sharing the challenge of getting people home safely, works. There are an increasing number of examples.
The second; Make discharge happen.
Discharge to assess. At first I though this was a risk, but it works. The patient is discharged and assessed in their own home. People manage better in their own home; assessment, practical aids and adaptations are done, right there and then. Aintree pioneered it.
Third; Bums off Beds.
Preventing the de-conditioning associated with being in bed, improves the chances of a speedier and safer discharge. Patients are ‘fitter’ and the demands on care packages, less. Initiatives like #endPJparalysis really do work.
Forth; Acute in the community.
Trusts working in the community in an ‘in-reach’ role, providing a support in the home, speeds discharge. It costs, but so do delayed transfers of care. Stockport have a great scheme.
I don’t see any changes in legislation until after the next election… goodness what that will bring. Right now the focus is on Brexit and clinging on. No money, no Parliamentary time and no appetite for structural change.
The NHS is this government’s orphan.
So… we’re on our own. We have to get on with it.
—————————-
Contact Roy – please use this e-address
roy.lilley@nhsmanagers.net
Know something I don’t – email me in confidence.
Leaving the NHS, changing jobs – you don’t have to say goodbye to us! You can update your Email Address from the link you’ll find right at the bottom of the page, and we’ll keep mailing.
———-
Disclaimer
Reproduced at thetrainingnet.com by kind permission of Roy Lilley.