It has a balletic quality.
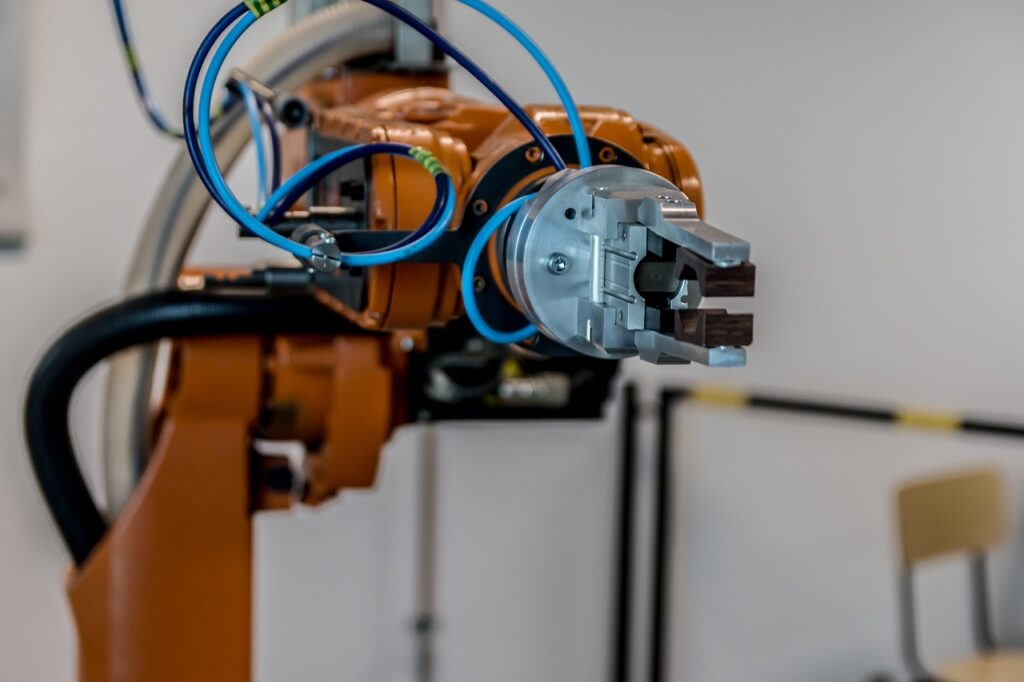
Orange arms sweep through the air with the precision of… of, well… a robot. Only a robot can be this accurate all the time, every time.
You should go. Visit the factory where the Mini is made. One is produced every 67 seconds.
There was a time when Mr Rolls and Mr Royce made cars… themselves. Highly skilled, component by component.
Henry Ford came a long… 1913, installed the first moving assembly-line for mass-producing the automobile. Reducing the time it took to build a car from more than 12 hours, to one hour and thirty three minutes.
He dismantled the skills and changed the processes. It was inevitable.
His people weren’t engineers. There weren’t enough of them.
It’s what has become a universal people issue. Not enough of the right people, in the right place at the right time to do the right job.
Assembly work was boring and relentless. Worker-turnover was high. Ford more than doubled their pay to $5 per day. They stayed and more workers flocked off the land, to the factories.
The inevitability of gradualness. Technology manipulating and manoeuvring. Insinuating its way into our lives.
Today, at the Mini factory, 350 different body parts are assembled by 280 robots. People, not required. In total, about 30,000 parts. Assembled, right-first-time. Some arriving, just-in-time… in 4 hours.
Better cars, made by fewer people. The inevitability of gradualness.
Look across most industries and services. Taking people out of the equation makes financial sense. Particularly in a world where there’s a global shortage of skilled labour.
The inevitability of gradualness. First comes the skill-shifting, then comes the machine… the robot.
QR codes on the table of restaurants. Meals delivered by a ‘server’. Banking, travel, shopping, local authority services… you don’t need me to spell it out. Work is changed.
And then… there’s the NHS…
… still plugging away. Trying to recruit care-staff in the midst of global shortages.
Hoping the pull of vocation will make up for the push-back from people who will not put up with heartless rota, miserable conditions, a perk-less, love-less grinding day. Pressured, bullied and messed about… 170,000 left last year.
A tin-eared government. Industrial relations at an all-time low.
However, a clue to the future beckoned in 2004.
The quality and outcomes framework, QOF, part of the GP contract, was introduced.
Paying GPs to carry out routine health checks… one component, taking a blood-pressure reading from pretty well everyone who turned up.
GPs couldn’t be bothered or were too busy. They trained receptionists to do it.
There was a row. Could a receptionist do it properly? That passed.
First the skill-shifting, then the machines.
Now, Williams Medical Supplies sell automatic BP measuring cuffs.
Patients, in the waiting room, do it for themselves. Technology… inevitable.
We never noticed, the slope got more slippery. We’d been oblivious to a US development. In 1960 the first physician associates appeared. Skill dismantling and shifting, big time.
Changing the fulcrum point of care. Easier and quicker to train and recruit.
A roll copied around the world.
The inevitability of gradualness.
The NHS ignored it. Stuck its fingers in its ears… sang La La.
In 2005, the UK Association of Physician Associates was established, as a professional body.
In 2006. DH+ commissioned an evaluation of the impact of PAs, which pointed to ‘great patient satisfaction’.
The Competence and Curriculum Framework was published. Royal Colleges gave PAs a free pass.
PAs, what do they do?
• medical histories
• physical examinations
• see patients with undifferentiated diagnoses
• chronic conditions
• formulate differential diagnoses
• diagnostic and therapeutic procedures
• develop and deliver treatment management-plans
• request and interpret diagnostics
• give health promotion and prevention advice
A lot of this’ll soon be done by machine learning, masquerading as Artificial Intelligence… particularly diagnosis…
… it’s the inevitability of gradualness.
PAs can’t prescribe. That’ll change. When nurses started prescribing some doctors said they’d poison everyone. They didn’t. Neither will PAs.
… it’s the inevitability of you-know-what.
The recognition that PAs should be regulated looks to be leading to the wholesale reform of regulatory processes… not before time…
… inevitable.
Yes, yes… I know, healthcare isn’t car making. It’s not banking nor fast food. Neither is it 1960.
Working in healthcare isn’t the love affair it once was. Politics, change, pressure, targets, ignorance, neglect… makes it something else.
In primary care the inevitable and gradual direction of travel has meant unregulated receptionists move from the clerical front-desk to the clinical front-line.
Care-guiding patients, the best they can, to see anyone but a Dr.
It’s a bad move. GIRFT recommends putting consultants at the front of the process in A&E. It’s safer and quicker and the outcomes are better.
Primary care is no different.
For the first go-around GPs should see everyone and it is they who should direct patients to allied professionals, prescribers, PAs, and diagnostic machines.
But, there aren’t enough GPs…
… Three in five GPs deliver more than the safe limit for patient contacts every day – and many routinely exceed it by double or more
… so, what to do? First the dismantling, then the skill shifting… then come the machines.
Bring on the robots… it’s inevitable.
News and Comment from Roy Lilley
Contact Roy – please use this e-address roy.lilley@nhsmanagers.net
Reproduced at thetrainingnet.com by kind permission of Roy Lilley.