There are three rules in BoJo’s Britain;
- Don’t fall sick,
- don’t get old,
- don’t be poor…
… now, there’s a fourth.
- Don’t fall over and phone for an ambulance.
That is not my conclusion and neither is it a criticism of the fabulous people who work in the service…
…it is my observation based on a report from the Association of Ambulance Chief Executives.
Thank you to the kind reader who sent it to me.
It was published in November 2021 and how I missed it, I don’t know. It looks like everyone missed it because it’s had no traction.
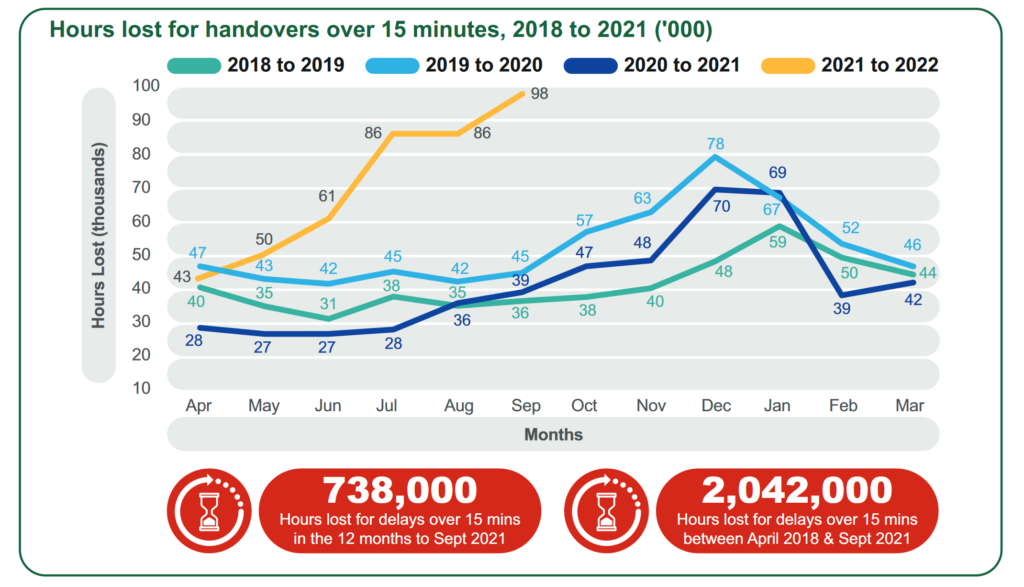
Have a look at the graphs that start on page eight.
I’d guess part of the problem is that for some bonkers reason, I cannot fathom, it is impossible to cut and paste from the report. So, it’s easier to stick it on a shelf than it is to circulate it. Basic error comm’s person.
However, let’s take it off the shelf…
…the review is about hand-over delays. The serious risks and harm they cause. Ambulance chiefs have taken a typical day and made reasonable extrapolations, to paint a picture of a Service in distress, acknowledging failure and asking for help.
No help has been forthcoming…
… if you are sick or injured and one of the 45% of ambulance customers who will need admission… the back of an ambulance is not the safest place to be.
Quite how many harmful ambulance handover delays there are, is a bit of a mystery.
There’s confusion and conflict in terms of ‘ownership’ of serious incidents, relating to handover delays. Which provider is it? Hospital or ambulance? Who is responsible for reporting and investigating?
Dunno…
That means ‘there is no recognition of the poor patient experience or potential harm caused as a result’…
… by the way, that’s a direct extract from the report.
On the 4th of January last year ambulance bosses counted 7,000 handover delays.
The report extrapolates those numbers into a horror story of waiting, in the back of a ‘van’, on a ‘bed’, not designed to be used for longer than about an hour, that will damage frail and elderly skin, with staff, who are fabulous, but not trained to do continuing-care. They do emergencies.
The more you read into the report, the more the story goes from disturbing to horror.
Vignettes of care and incidents… there are plenty to choose from. Eight out of ten of those experiencing handover delays were assessed as experiencing ‘harm’ and one in ten, ‘serious harm’.
An ambulance is not as safe as you thought it was.
Certainly not for the patient with red-flag sepsis, very high on the NEWS2 score of ten (meaning pull yer finger out and sort this person, now), waiting an hour and 28 minutes, without life-saving antibiotics.
There are many more horrors like this.
Usually, you can’t get organisations to dig out their failures. Here the ambulance services have done it in spades. With a JCB.
The Ambulance Service cries for help included…
…calling on the CQC ‘to include hospital handover delays in their inspections of local health systems.’
Inspection’s a waste of time, we know that.
They wanted the Health Service Investigation Bureau to undertake an independent thematic review.
They didn’t.
The NHS Long Term Plan sets out a ‘vision to eliminate ambulance handover delays’.
It’s not happened.
Guidance was issued as far back as 2012.
We are still in a mess.
Ambulance bosses thought ‘new metrics of performance’ might be a solution.
That’s code for a category fiddle like there is now with 999 calls. Lying on the cold kitchen floor, for hours, with a broken hip is not Category 1.
The cherry on the cake is this revelation;
‘Senior level discussions about how to prevent handover delays have been taking place for years… [attempts at] implementing improvement measures to address the issues… [failed and] the problem persists.’
The latest numbers; During the week ending 20 February, there were 7,200 over 60 minutes and over 15,000 delays, over 120 minutes in January 2022.
The best NHSE/I could manage was a foot-stamping, billet-doux to Trusts, instructing them to ‘immediately stop all ambulance handover delays’.
They haven’t.
This report is a harrowing plea to get the issue on the table. Asking for help and the response is a massive failure of the NHSE/I Board.
There is no ambulance representative on the NHSE Board. Why? Because it would bring the problem too close for comfort…
… and that would prick the NHSE Board’s bubble of love and fabulousness…
… and deliver a dose of reality that would send them all home in tears, before teatime.
———
PS: Since writing this I’ve heard; ‘West Mids ambulance under instructions from NHSE/I, had a regional meeting Monday night and agreed that from 8.15pm Monday, ambulances are to drop patients off at A&E – waiting no longer than 20 mins!’ … that is bound to help.
News and Comment from Roy Lilley
Contact Roy – please use this e-address roy.lilley@nhsmanagers.net
Reproduced at thetrainingnet.com by kind permission of Roy Lilley.